A trial supported by the Translational Research Center for Medical Innovation (TRI) aims to establish best practices for clinicians performing colon cancer surgery1.
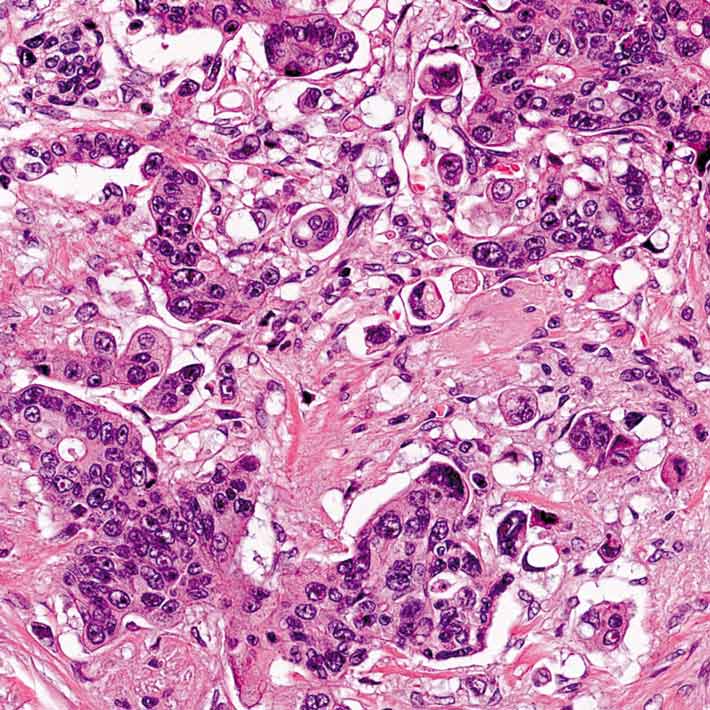
Survival outcomes for patients with early-stage colon cancer depend heavily on the quality of surgery they receive. Yet there are no international standards for how best to remove a cancerous colon along with the nearby lymph nodes, through which tumor cells may spread. Excise too much tissue, and patients may experience postoperative complications. Remove too little, and the cancer may recur. Known as T-REX, the Japanese study is designed to find the optimal level for patients and surgeons everywhere.
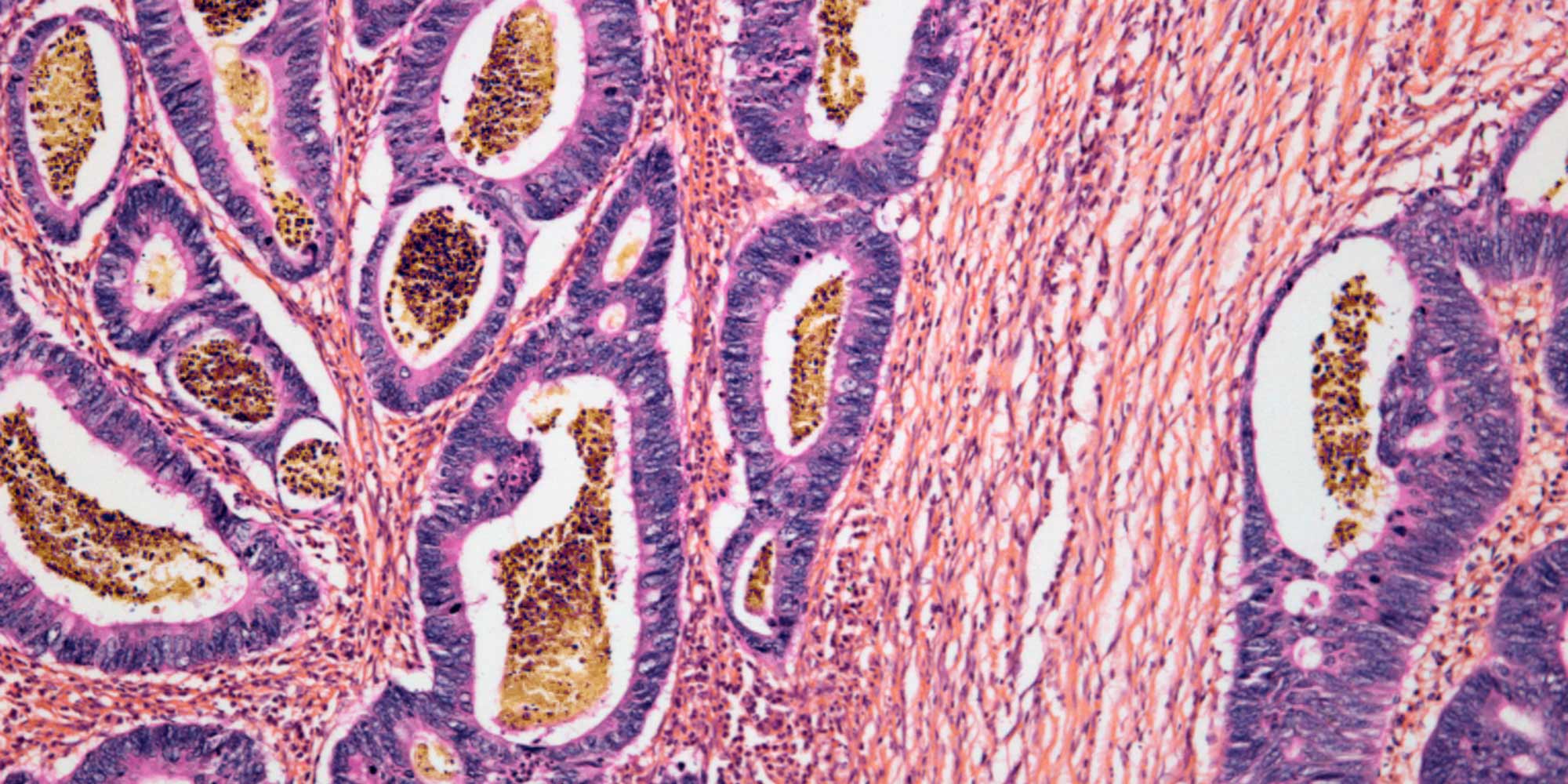
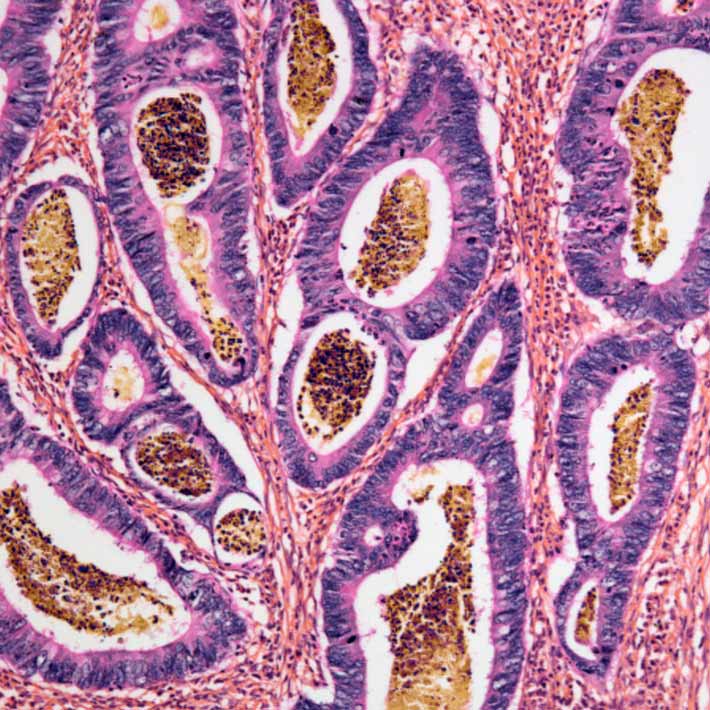
About 4,000 patients who are undergoing bowel resection in Japan, South Korea, Germany, Russia, Lithuania and Taiwan are enrolled in T-REX. For each patient, the researchers took high-resolution digital photographs of the excised tissue immediately after surgery. They then mapped the distribution of lymph nodes and feeding arteries to determine the optimal amounts of colon and surrounding tissue to remove.
The trial data is currently being analyzed, but Hideki Ueno, a trial leader from the National Defense Medical College in Tokorozawa, Japan, and his colleagues are optimistic about the outcome. “We anticipate the findings will strongly influence colorectal surgeons around the world and will serve as a cornerstone for establishing optimal surgical practices for colon cancer,” Ueno says. “In particular, the unprecedented level of detailed mapping of supplying arteries and lymph nodes in the study will help surgeons to understand the risk areas of lymphatic metastasis.”
The motivation for the T-REX protocol came from a 2013 symposium sponsored by TRI, where researchers from the United States, Europe and Asia presented their operative procedures for treating colon cancer. Japanese clinicians have long relied on the so-called 10-centimeter rule — to cut about a baseball’s length from the tumor edge, but no such unified practice is common in Western countries, where surgeons tend to remove different amounts of tissue depending on how much blood is supplied to the colon.
“At the symposium, we recognized there was great variability in surgical treatments for colon cancer,” says Kenichi Sugihara from Tokyo Medical and Dental University, who organized the event and is helping to lead the T-REX study. “Furthermore, we realized we needed international collaboration to establish a global standard of optimal surgery for colon cancer.”
Ueno, Sugihara and their colleagues outlined the study protocol and trial aims in November in the Japanese Journal of Clinical Oncology.
References
- Shiozawa, M., Ueno, H., Shiomi, A., Kim, N. K., Kim, J. C., Tsarkov, P. et al. Study protocol for an international prospective observational cohort study for optimal bowel resection extent and central radicality for colon cancer (T-REX study). Japanese Journal of Clinical Oncology hyaa115 (2020). | article
About the Researcher

Kenichi Sugihara, Professor, Tokyo Medical and Dental University
Kenichi Sugihara's research interests include the
optimal scope of lymph node dissection for colon cancer and rectal cancer,
adjuvant chemotherapy based on risk of recurrence after curative surgery for
colon cancer and peri-operative chemotherapy for multiple liver metastases from
colorectal cancer.
Tokyo Medical and Dental University

Hideki Ueno, Professor of Surgery, National Defense Medical College
Professor Ueno's research is focused on
surgical pathology and the personalized treatment of colorectal cancer.