Transplanting cells from inside the mouth to the eye’s surface has had remarkable success in restoring sight, but high costs of the therapy could restrict widespread application.
For nearly 20 years, Chie Sotozono, head of the Department of Ophthalmology at the Kyoto Prefectural University of Medicine, has been using transplantation to help patients with a specific group of eye conditions known as severe ocular-surface diseases.
These diseases affect the cornea — the transparent layer covering the eye’s surface. They can be caused by injury such as burns or a reaction to medications, but can also be the result of immune system disorders such as Stevens–Johnson syndrome, or the loss of the stem cells that normally repair and maintain the corneal surface.
The consequences of these diseases can be devastating. “The patients were unable to read or even walk without aids,” Sotozono says.
Treatment options for these diseases are limited, especially once they are more severe. Research has focussed on using transplanted cells and membranes to combat the inflammation causing damage and provide a scaffold for the cornea to rebuild itself.
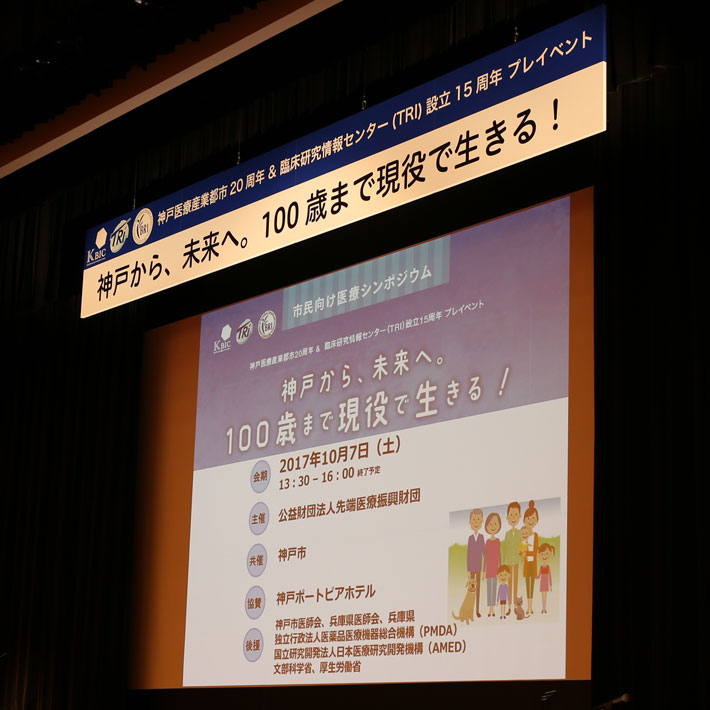
Sotozono’s team has been treating severe corneal diseases by combining transplanted cells from inside the mouth with a piece of amniotic membrane, which encases a foetus and placenta inside the womb. More recently she has partnered with researchers from the Translational Research Informatics Center to investigate whether stem cells harvested from the lining of the mouth might also work for these patients.
In a study involving 40 patients with severe ocular-surface disease, Sotozono and colleagues collected sheets of cells from the inside cheek of each patient, and transplanted those to the surface of the cornea1. Some patients also received transplanted amniotic membrane at the same time.
The results were astounding, with most patients recovering some, if not most, of their sight.
“We were ecstatic by the results,” Sotozono says. “They can now read, walk, eat by themselves, and attend school or have a career: a truly improved quality of life.”
With few other treatments available for severe ocular-surface diseases, Professor Sotozono hopes this approach could make a big difference to the lives of people around the world. The challenge will be delivering it.
They can now read, walk, eat by themselves, and attend school or have a career: a truly improved quality of life
“The costs of making the regenerative-medicine product are high, and the profitability is sometimes low,” Sotozono says. “We hope that the social systems needed to support innovative regenerative medicine will continue to improve, which would expand practical clinical uses worldwide.”
References
- Sotozono, C. et al. Visual improvement after cultivated oral mucosal epithelial transplantation. Ophthalmology 120, 193–200 (2013). | article
- Sotozono, C. et al. Predictive factors associated with acute ocular involvement in Stevens-Johnson Syndrome and toxic epidermal necrolysis. American Journal of Ophthalmology 160, 228–237 (2015). | article
- Sotozono, C. et al. Cultivated oral mucosal epithelial transplantation for persistent epithelial defect in severe ocular surface diseases with acute inflammatory activity. Acta Ophthalmologica: 92, e447–e453 (2014). | article
About the Researcher

Chie Sotozono, Chair of the Department of Ophthalmology, Kyoto Prefectural University of Medicine
Professor Chie Sotozono is a world-renowned expert in the treatment of severe ocular-surface disorders, especially Stevens–Johnson syndrome, and specializes in clinical research, cornea-related diseases, and groundbreaking new pathways of regenerative medicine.
Department of Ophthalmology, Kyoto Prefectural University of Medicine