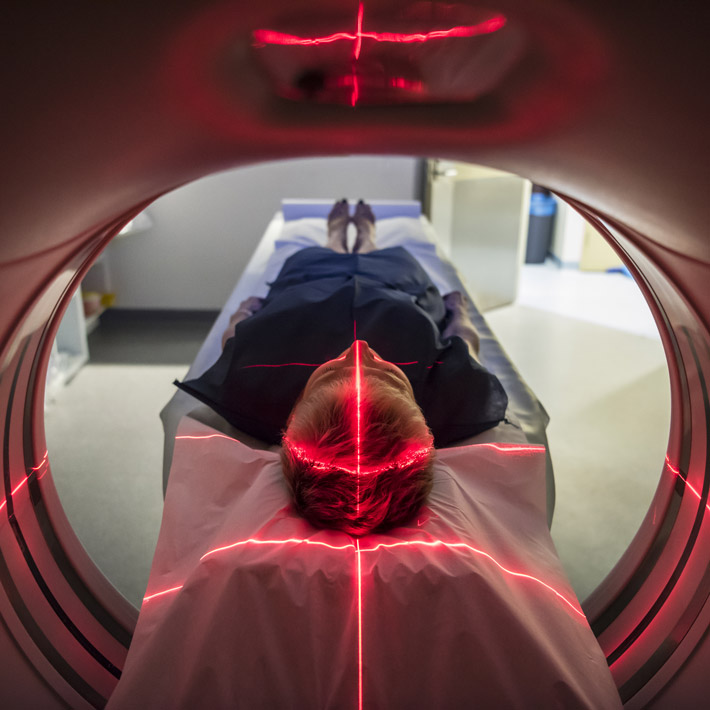
Approximately one in five people with cancer have a ‘rare’ version with an incidence of less than six cases per 100,000 people per year. Such cancers are associated with worse survival rates than more common cancers partly because they are harder to diagnose. A study led by Toshirou Nishida at the National Cancer Center Hospital in Tokyo shows that consulting specialized pathologists can improve the accuracy of rare cancer diagnosis and, potentially, patient outcomes.
Emerging knowledge about the genetic and molecular mechanisms underpinning rare cancers is important for diagnosis and selecting the best treatment. Nishida and colleagues from the Translational Research Center for Medical Innovation (TRI) and hospitals across Japan, examined the agreement between rare cancer diagnoses made locally by general pathologists and by disease-specific pathologists in central laboratories, and the impact of the results on treatment decisions.
Between 1,500 and 2,000 new cases of gastrointestinal stromal tumour (GIST), a cancer that usually originates in cells lining the gastrointestinal tract, are diagnosed in Japan each year. Surgery is the only potential cure for GIST, but almost 40 per cent of patients experience disease recurrence after complete removal of the tumour.
In 80-90 per cent of GIST cases, tumour growth is driven by mutations in the genes coding the cell-surface receptor KIT or platelet-derived growth factor receptor A (PDGFRA), which lead to unregulated cell proliferation. Upon identification of these mutations by immunostaining or genotyping, the cell growth inhibitors imatinib are routinely used as to prevent tumour recurrence after surgery.
Nishida and colleagues examined data from 534 patients with high-risk GIST diagnosed and treated in participating hospitals between 2012 and 2015. After surgery, 81 per cent of patients received imatinib.
When patient tumour samples were genetically sequenced and pathologically examined by central GIST specialists, 19 cases (3.6 per cent) were diagnosed as non-GIST and 93 (18.1 per cent) were reclassified into lower risk categories. “This small but significant discordance suggests that specialized pathological examination should be sought to confirm the diagnosis of high-risk GIST” says Nishida.
Because imatinib is not effective in non-GIST patients or patients bearing a particular PDGFRA mutation, the authors investigated whether treatment was discontinued in light of the new diagnoses. Available data indicated that imatinib use was stopped in only 6 out of 10 non-GIST patients and in 5 out of 8 patients with a treatment-resistant PDGFRA mutation. “Our findings suggest that GIST guidelines may need to be refined to facilitate treatment changes in local hospitals following central pathology results” explains Nishida.
Future studies will evaluate the effect of these inconsistencies on patient outcomes and determine whether diagnosis of other rare cancers could also be improved by seeking confirmation by specialized pathologists.
References
- Nishida, T. et al. Adherence to the guidelines and the pathological diagnosis of high-risk gastrointestinal stromal tumors in the real world. Gastric Cancer advance online publication, 30 April 2019 (doi:10.1007/s10120-019-00966-4). | article
About the Researcher
Toshirou Nishida, Director, National Cancer Center Hospital
Dr Toshirou Nishida is Director of the
National Cancer Center Hospital. He also works as a surgical oncologist in the
Department of Gastric Surgery of the Hospital and is an internationally recognized
expert in gastrointestinal stromal tumour (GIST).
Dr Nishida is involved in clinical studies and
translational research projects investigating the underlying mechanisms of GIST
through genomic studies of patient samples. He is particularly interested in improving
disease management and the quality of life of patients with rare cancers.
Department of Gastric Surgery, National Cancer Center Hospital