Clinical trials that test the safety and efficacy of new drugs and therapies are the cornerstone of medical research. However, these trials are typically limited to small groups of selected patients. To better reflect the real world, clinical researchers are increasingly looking for more comprehensive data.
This daunting topic was tackled at the Third Global Academic Research Organization (ARO) Network Workshop in Tokyo on 7 March 2018. Discussing the development of an online ‘data commons’ for childhood cancers, Samuel Volchenboum of the University of Chicago revealed the scale of ambition, describing the ultimate goal as being able to collect “all data, from all patients, at all times.”
In particular, participants looked at the potential for worldwide data networks for rare cancers and for amyotrophic lateral sclerosis (ALS) — a debilitating and incurable disease in which the neurons involved in controlling voluntary muscle movement progressively die, leading to paralysis and ultimately death. ALS was made prominent by the late cosmologist Stephen Hawking, who suffered the disease.
“All data”
One key barrier to obtaining more data, according to Jacques Demotes of the European Clinical Research Infrastructure Network (ECRIN), is that permission is often only given by patients for their data to be used within the scope of a single trial. This represents huge waste, he pointed out. Demotes outlined ten principles developed at the ECRIN to help clinicians ethically overcome this structural issue, ranging from providing incentives for data sharing and obtaining explicit broad consent, to using common data and metadata standards.
“From all patients”
Chung Hsu of the China Medical University and Healthcare System talked about recent changes in Taiwan’s health system which has moved beyond pooling data from multicenter clinical trials, to using big data from all accessible patients. Hsu listed an impressive array of outcomes, including studies that drew links between hypertensive disorders during pregnancy and strokes; studies that linked varicose veins and the occurrence of more serious vascular diseases; and work that looked into the correlation between the sedative, zolpidem, and cancer risk.
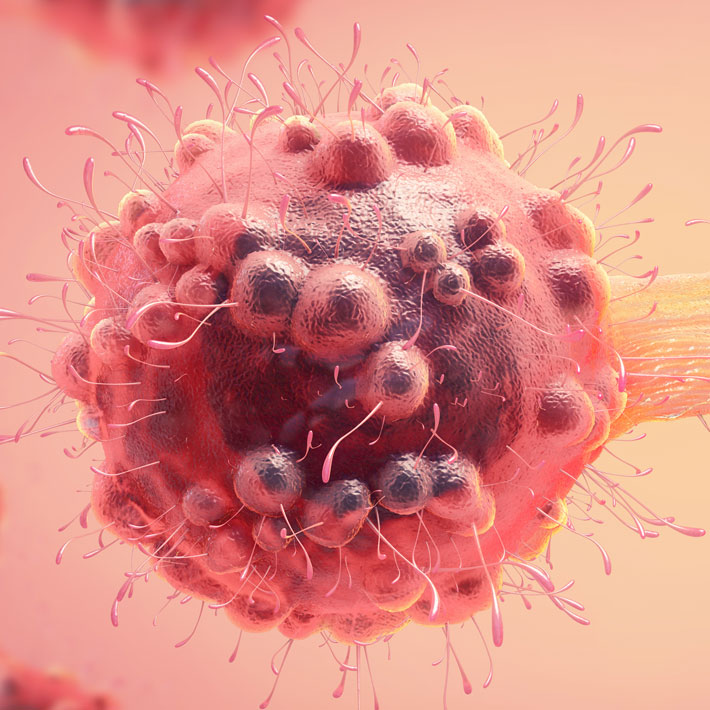
Seung Hyun Kim of Hanyang University, described a nationwide ALS registry established in South Korea. He explained that by law, relevant data from the national health insurance system had previously been inaccessible to clinicians, but that this had changed last year. He talked about one of the outcomes of his team’s access to this new data: a new stem-cell treatment for ALS, which involves taking stem cells from a patient, cultivating them outside the body, and then injecting back into the patient. While the treatment does not replace damaged or destroyed neurons, it does protect healthy ones.
Shin-ichi Muramatsu of Jichi Medical University, Japan, described a new gene-based therapy for ALS. It uses a virus to transfer genes into a patient to increase the local production of dopamine, which helps to control motor function. Muramatsu showed a video of a 15-year-old patient who, after being unable to get out of bed, was able to transport himself some six months after receiving an injection of the virus.
“All the time”
The logistics involved in following up with patients after the limited period of a trial is another major hurdle, noted Gen Sobue of Nagoya University. He described how he has overcome this by holding phone interviews with ALS patients every three months.
Global big data
The global scale of this year’s workshop was a logical progression of the scope of past workshops. The first focused on developing Japan-wide networks, the second looked at Asian networks, while this workshop emphasized making global connections.
In closing the workshop, Norihiro Sato from Hokkaido University, Japan, emphasized the value of big data and data-sharing transcending national boundaries, and he expressed hope that the workshop had helped establish the foundations of bigger global data networks.