New insights into the effects of the cholesterol-lowering drug, pravastatin, on blood vessel narrowing and ‘bad’ cholesterol-levels have been gleaned through further analysis of the Japan Statin Treatment Against Recurrent Stroke (J-STARS) study data.
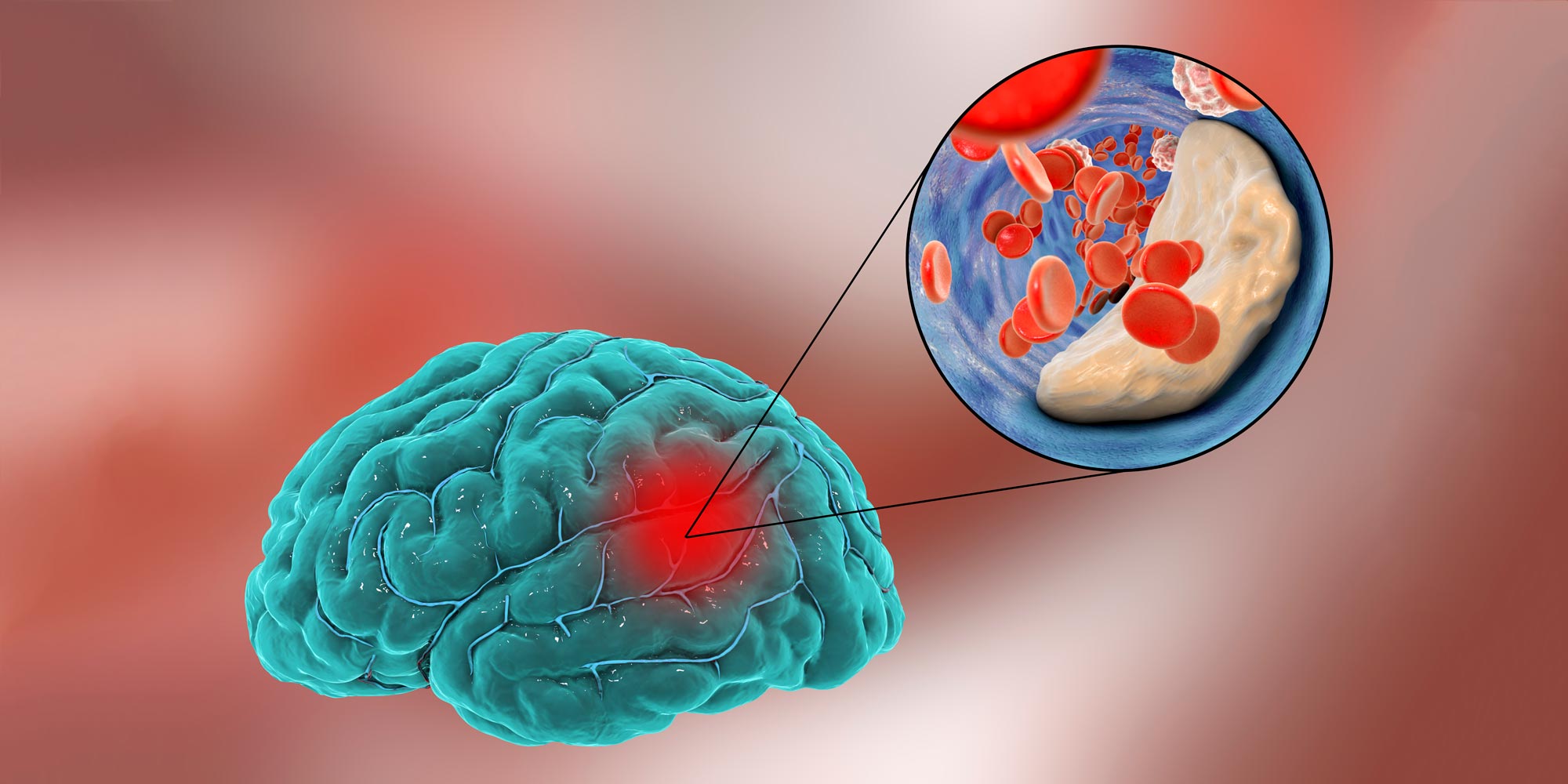
In 2015, the J-STARS study showed that 10 milligrams per day of pravastatin prevents the recurrence of atherothrombotic brain infarction, one of the most common types of stroke, in Asian patients1.
Despite the widespread use of statins to reduce low-density lipoprotein (LDL), or ‘bad’ cholesterol, and prevent cardiovascular events, there is little information regarding racial differences in response to statins. East Asian populations have a higher incidence of intracerebral hemorrhage than Western populations and because lowering cholesterol too much could increase the risk of intracerebral hemorrhage, Asian populations are administered three to four-fold lower doses of statins.
A study led by Masatoshi Koga, at the National Cerebral and Cardiovascular Center in Osaka, used ultrasound to examine the effect of five-year pravastatin treatment on the thickness of the inner two layers of the carotid artery, the intima and the media, a reliable surrogate marker for atherosclerosis, or blood vessel narrowing2.
“In patients with high stroke risk, long-term pravastatin treatment reduced progression of carotid intima-media thickness, indicating that pravastatin may be beneficial to reduce the progression of atherosclerosis and subsequent cardiovascular events”, explains Koga.
Another study, led by Naohisa Hosomi at Hiroshima University, used J-STARS data to determine the LDL cholesterol levels associated with a lower risk of stroke recurrence3.
They found that irrespective of statin treatment, patients with LDL cholesterol levels of 80 to 100 milligrams per decilitre had a lower risk of stroke recurrence. Surprisingly, the effect of pravastatin on preventing atherothrombotic brain infarction was not associated with LDL cholesterol levels, suggesting that the drug is working through other mechanisms to reduce the recurrence of this type of stroke.
Also, irrespective of pravastatin treatment, patients with LDL cholesterol levels of 100–120 milligrams per decilitre had a significantly lower risk of lacunar infarction, a type of stroke that occurs when blood flow to one of the small arteries deep within the brain becomes blocked.
“These findings suggest that the outcome of statin treatment is only partly dependent on the decrease in LDL levels achieved and that the desirable target LDL levels for preventing stroke recurrence may be different for different stroke subtypes”, says Hosomi.
Further research into the effects of statins and other cholesterol lowering agents will contribute to optimize the regulation of LDL and prevent stroke recurrence in Asian patients.
References
- Hosomi, N. et al. The Japan Statin Treatment Against Recurrent Stroke (J-STARS): A multicenter, randomized, open-label, parallel-group study. EBioMedicine 2, 1071–1078 (2015). | article
- Koga, M. et al. Long-term effect of pravastatin on carotid intima-media complex thickness: The J-STARS echo study (Japan Statin Treatment Against Recurrent Stroke). Stroke 49,107–113 (2018). | article
- Hosomi, N., et al. Desirable low-density lipoprotein cholesterol levels for preventing stroke recurrence: A post hoc analysis of J-STARS study (Japan Statin Treatment Against Recurrent Stroke). Stroke 49, 865–871 (2018). | article
About the Researcher

Masayasu Matsumoto, Adviser, Sakai City Medical Center, Sakai City, Osaka, Japan
Dr Masayasu Matsumoto is a professor emeritus of Hiroshima University, has been working as a director of Hoshigaoka Medical Center since 2015 and as an adviser of Sakai City Medical Center since April 2018. He is an active member of the World Stroke Organization’s board of directors. In 1976, he graduated from Osaka University and after training in clinical neurology, carried out several clinical and basic research studies on Stroke Neurology at Osaka University, the Mayo Clinic and Hiroshima University. He was also involved in several stroke registry and intervention studies such as REACH, JSSRS, HARP, CSPS, PROGRESS, JAST, J-ROCKET AF, J-PPP and J-STARS.

Masatoshi Koga, Director, Department of Cerebrovascular Medicine, National Cerebral and Cardiovascular Center
Masatoshi Koga is currently the director of the Department of Cerebrovascular Medicine, National Cerebral and Cardiovascular Center in Japan. He spent two years as a Research Fellow at the National Stroke Research Institute in Melbourne, Australia. His main research interests are management of acute stroke, ultrasound and secondary prevention.
National Cerebral and Cardiovascular Center in Osaka

Naohisa Hosomi, Associate Professor, Department of Clinical Neuroscience and Therapeutics, Hiroshima University Institute of Biomedical & Health Sciences
Naohisa Hosomi is an associate professor at the Department of Clinical Neuroscience and Therapeutics, Hiroshima University Institute of Biomedical & Health Sciences, Japan. He trained at Kagawa Medical University and spent two years as a Research Associate in the Department of Molecular and Experimental Medicine at The Scripps Research Institute in California, USA. He has published over 140 research papers and serves on the Board of the Japanese Society of Hypertension and of the Japanese Society of Neurology. His main research interests are in hypertension, atherosclerosis and stroke.
Hiroshima University Graduate School of Biomedical & Health Sciences