Transplanting stem cells from the patient’s own blood could be a safe and effective enhancement to treating fractures that fail to heal, say researchers associated with the Translational Research Center for Medical Innovation (TRI) in Japan. They have described this phenomenon in the TRI publication Principles of Regenerative Medicine.
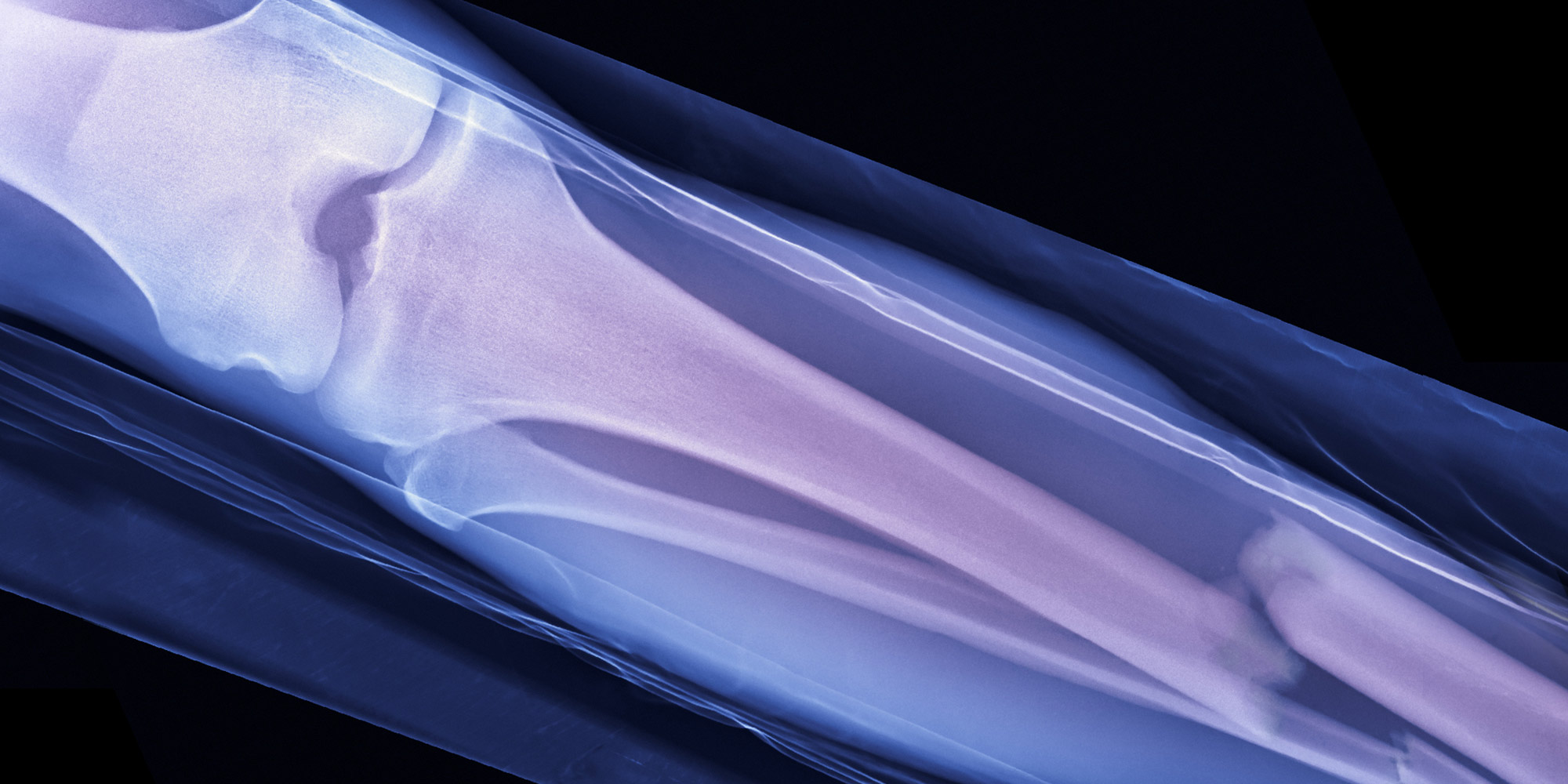
Usually, a fractured bone will heal by itself if it is simply immobilized. But between 5% and 10% of bone fractures fail to heal, even after bone grafting, partly because of inadequate circulation at the fracture site. Even the use of stem cells from bone marrow has been of limited effectiveness in healing these non-union fractures.
The success of endothelial progenitor cells (EPCs) in treating tissue damage due to poor blood supply prompted Ryosuke Kuroda of Kobe University Graduate School of Medicine and colleagues to investigate their usefulness in treating non-union fractures.
That’s because restoring blood circulation to the site of fracture is understood to be essential to healing. New blood vessels were thought to develop in adults through the proliferation and migration of endothelial cells from the lining of nearby blood vessels. It is now known that a second mechanism, previously considered to occur only in the fetus, also contributes to blood vessel formation. EPCs, which are abundant in bone marrow, are released into the blood and carried to the site of damaged tissue, where they proliferate and differentiate to form new blood vessels.
In animal studies conducted by the researchers, EPCs increased in the bone marrow and peripheral blood after fracture. Intravenous transplantation of EPCs showed that they accumulated at the non-union site and contributed to fracture healing by stimulating bone growth and the formation of new blood vessels. Two weeks after transplantation, the EPCs had differentiated into mature endothelial cells and bone-forming cells at the fracture site. After 2 months, all fractures in animals in the treated group had healed. These results suggested that local transplantation of EPCs would be useful as a new treatment option for non-union fractures.
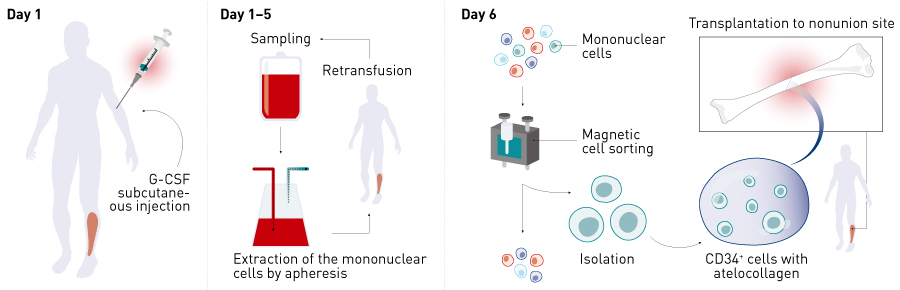
The researchers tested the concept on seven patients with non-healing leg fractures, who underwent both bone grafting and transplantation of EPCs drawn from their own blood. Twelve weeks after surgery, X-ray images showed that 71% of fractures had healed. In contrast, healing occurred in only 18% of patients with non-healing fractures who had only a bone graft and no EPC transplantation. The average time taken to heal was 16.1 weeks in the EPC-treated group, compared with 29.1 weeks in the non-EPC group. No serious adverse events were reported 1 year after surgery. A multicenter study in a larger number of patients is currently being conducted.
Kuroda and team believe that, unlike conventional therapies, EPC therapy regenerates both bone and blood vessels for non-union fractures.