Using stem cells as part of first-line therapy for heart attack has the potential to speed up the healing process and improve the long-term outlook for patients.
An acute myocardial infarction (AMI), or heart attack, is caused by a sudden blockage of a coronary artery supplying the heart muscle. The resulting lack of blood flow leads to the death of some heart muscle tissue, known as an infarct. Following an AMI, changes occur in the structure of the heart that reduce cardiac function and can later lead to heart failure.
Shinya Minatoguchi from Gifu University Graduate School of Medicine and colleagues are researchers associated with the Translational Research Center for Medical Innovation (TRI) in Japan. They have made significant progress towards the goal of using stem cells that can differentiate into heart muscle cells known as cardiomyocytes, and grafting these into the damaged muscle.
The existence of multilineage-differentiating stress enduring (Muse) cells was first proposed in 2010. These cells, which may have the ability to differentiate into any cell type, are thought to reside in bone marrow, skin, adipose tissue, connective tissue of various organs and blood.
Minatoguchi and co-workers found that the number of Muse cells in the blood increased after an AMI. They also observed that the more damaged the heart muscle was, the more Muse cells were released into the blood. A larger increase in Muse cells during the acute phase was associated with improved cardiac function and less change in heart structure 6 months later.
These results suggested that administering Muse cells during the acute phase of AMI could improve cardiac function and reduce the damaging changes in heart structure that can lead to heart failure.
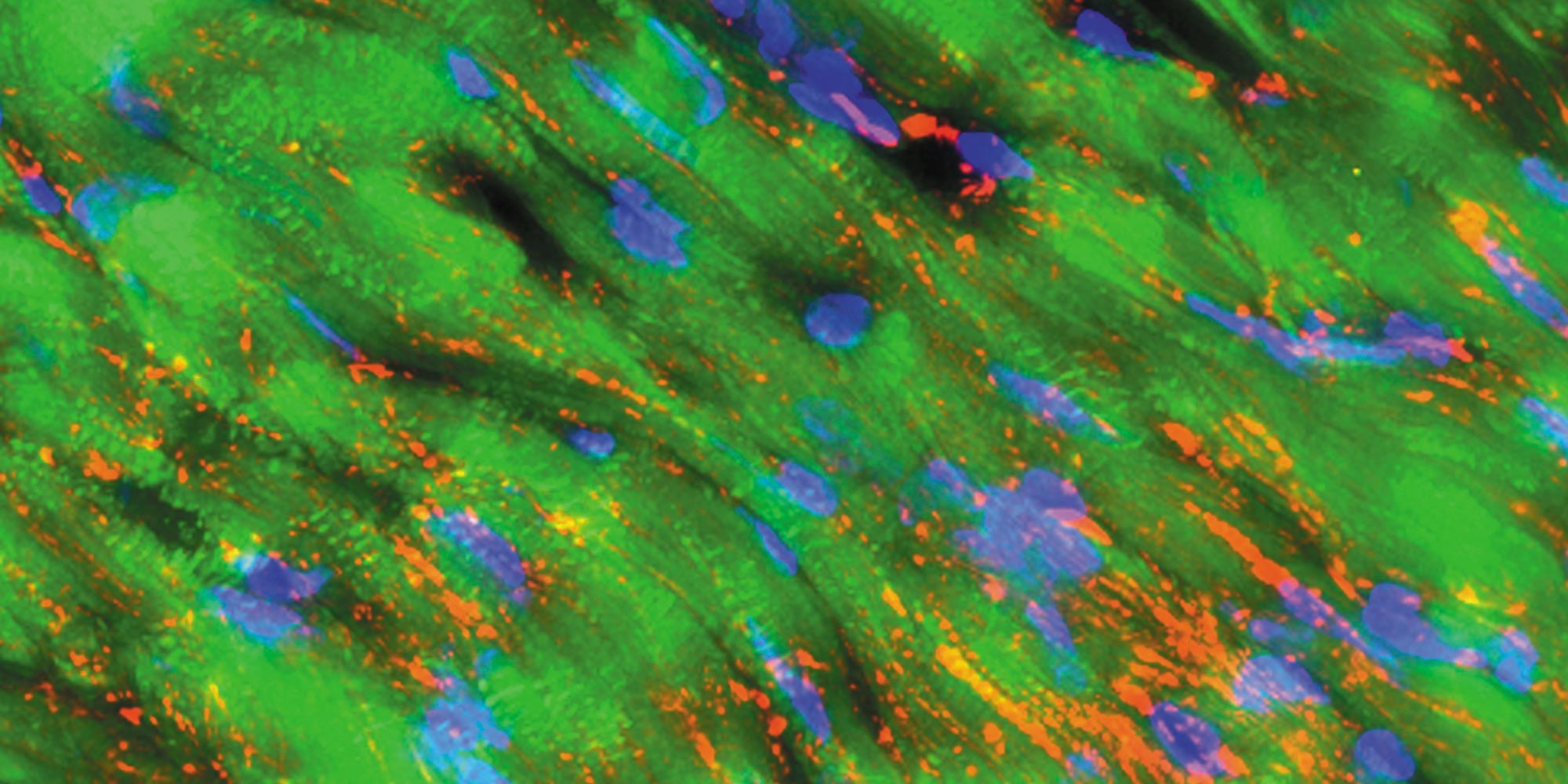
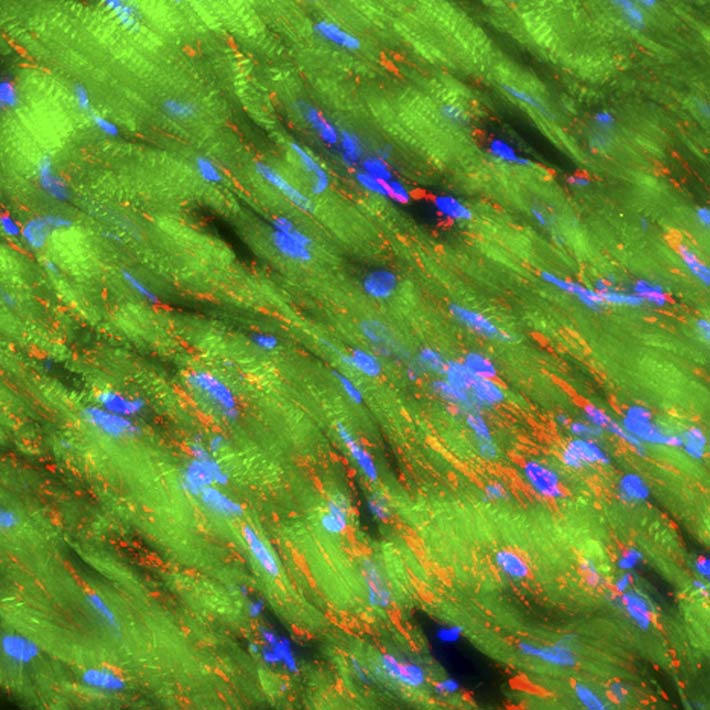
Minatoguchi’s and Dezawa’s teams confirmed the ability of Muse cells to differentiate into cardiomyocyte-like cells in cell culture. In animal models of AMI, Muse cells preferentially grafted into the damaged tissue, differentiating into functional cardiomyocytes and also forming blood vessels. Infarct size was reduced as were changes in heart structure, and heart function improved. Muse cells seemed to be twice as effective as conventional stem cells from bone marrow in reducing infarct size. Because of their immune markers, Muse cells are not rejected and hence persist after engraftment.
These results suggest that treating AMI using Muse cells could be more effective than current first-line therapy. Using the patient’s own cells is not practical as at least a week is needed to isolate and culture sufficient cells for treatment. But using Muse cells from another animal proved equally effective in reducing infarct size and improving cardiac function. Clinical trials to test this approach are ongoing.