Preliminary results from the world’s largest prospective cohort study, a nationwide study of prostate cancer treatment in Japan, demonstrate the value of ongoing, high-quality professional training and long-term monitoring of patients.
The continuing Japanese Prostate Cancer Outcome Study of Permanent Iodine-125 Seed Implantation (J-POPS) began in 2005. It aims to evaluate the long-term safety and efficacy of brachytherapy, a form of radiotherapy, using permanent iodine-125 seed implantation (PI) for prostate cancer.
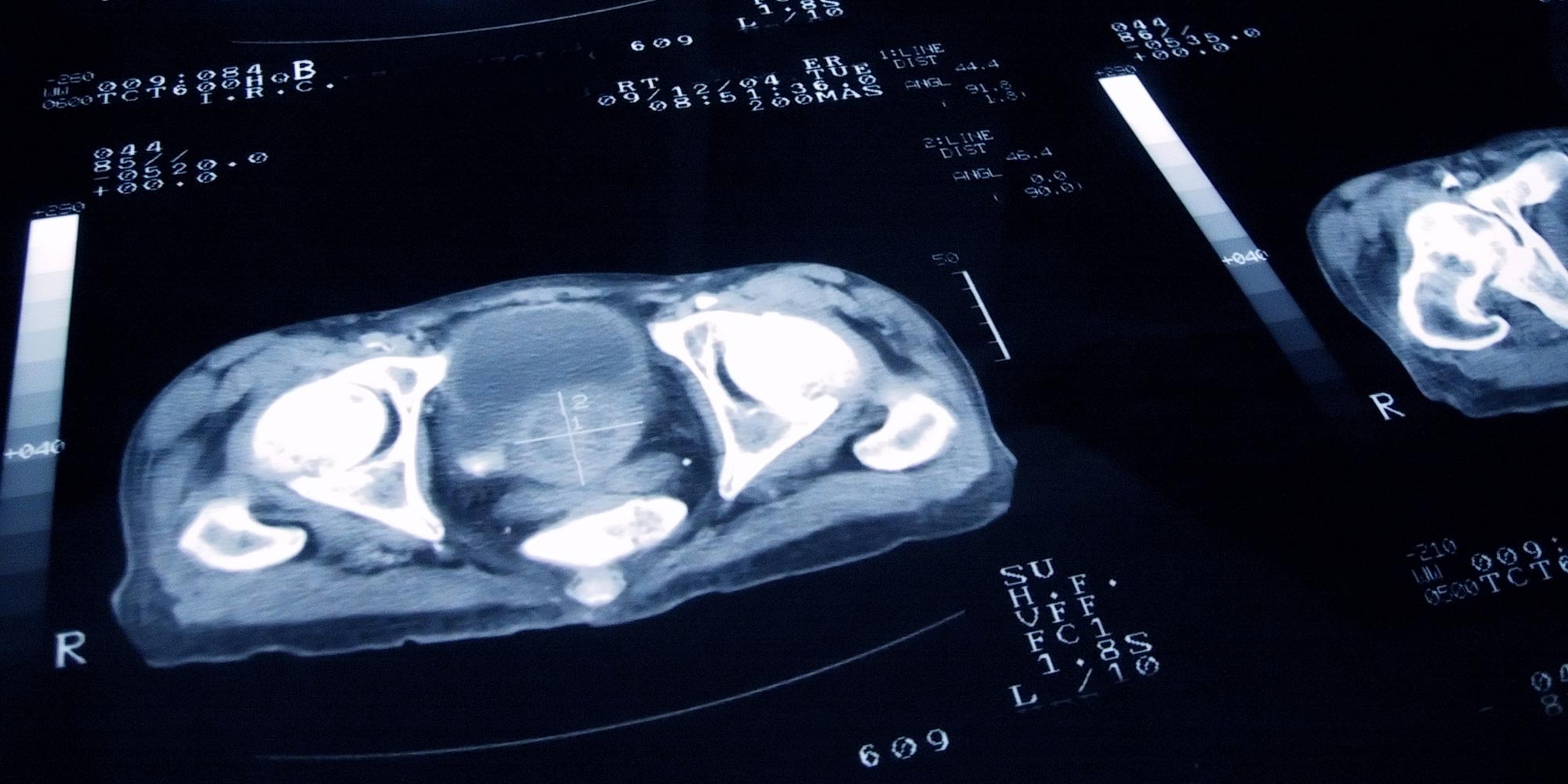
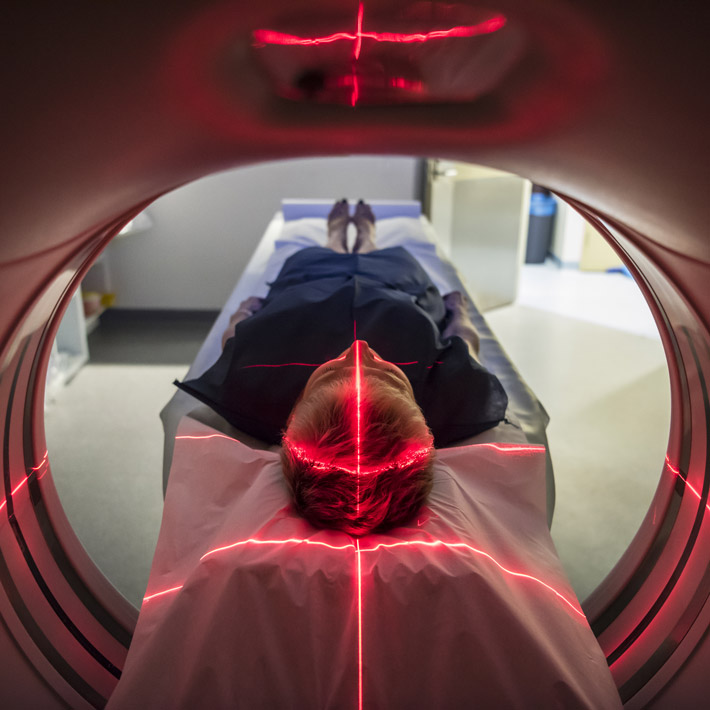
Prostate brachytherapy involves the injection of sealed radiation sources, or ‘seeds’, directly into the body at the tumor site. The technique allows high doses of radiation to be targeted so precisely that surrounding tissues and bodily fluids remain largely unaffected. The procedure requires just one day of hospitalization, followed by a month of medical care.
“The J-POPS study now includes 40 per cent of all patients receiving PI treatment across Japan, providing an excellent source of data,” says Kazuto Ito at Gunma University, Japan. “Maintaining excellent PI treatment skills in individual institutions is challenging. Our approach, which includes extensive, ongoing staff training for all J-POPS registered institutions, reduces the likelihood of selection bias and publication bias in our results.”
Ito’s team analyzed data from 2,316 patients — 45.2 per cent classified as low risk, 54.8 per cent as intermediate/high risk — who were registered with J-POPS between 2005 and 2007. Their results suggest that J-POPS’ rigorous quality control has contributed to a relapse-free survival rate of around 90 per cent and an overall survival rate of 97 per cent five years after initial treatment — of the patients that did not survive, only 7 died of prostate cancer.
A key issue explored by the study was how best to monitor levels of prostate-specific antigen (PSA), which rise during prostate cancer. Doctors closely monitor PSA levels in PI patients to look out for treatment failure — defined when PSA levels rise above a threshold known as the Phoenix definition. However, the J-POPS researchers believe that the Phoenix definition might not capture accurate results, particularly for younger men.
“When using the Phoenix definition, it was difficult to exclude those patients experiencing a temporary PSA increase, which can occur as a result of testosterone recovery,” says Ito. “The Phoenix definition mislabeled this benign PSA ‘bounce’ as PSA failure, especially in younger men. We have defined a new J-POPS definition to attempt to take this PSA bounce into account.”
The team will continue analyzing PSA failure using further data, and will examine whether the J-POPS definition provides a more rigorous method for identifying patients at risk of relapse and metastasis.
“Our success in maintaining nationwide PI quality could be an ideal model for all remaining countries where PI has not yet been introduced,” says Ito.
References
- Ito, K., Saito, S., Yorozu, A., Kojima, S., Kikuchi, T. et al. Nationwide Japanese prostate cancer outcome study of permanent iodine-125 seed implantation (J-POPS): First analysis on survival. The International Journal of Clinical Oncology, published online 22 June 2018 (doi: 10.1007/s10147-018-1309-0). | article
About the Researcher

Kazuto Ito, Director, the Institute for Preventive Medicine, Kurosawa Hospital
Kazuto Ito, MD, PhD, is currently the director of the Institute for Preventive Medicine, Kurosawa Hospital following 12 years as an associate professor in the Department of Urology at Gunma University Graduate School of Medicine, Japan. Ito graduated from medical school at Gunma University and conducted research at the Erasmus Medical Centre, Rotterdam, Netherlands, between 2002 and 2003. He was selected as a scholar of the American Urological Association–Japanese Urological Association Academic Exchange Program and, in 2010, worked at the University of California, San Francisco, USA. His research interests include prostate cancer epidemiology, screening and biomarkers, including PSA and related factors, minimally invasive surgery and radiation therapy for urological cancer. Ito has served on the Editorial Board of European Urology since 2008 and was one of the 2017 Reviewers of the Year for European Urology.